Aortic Dissection
Summary
Aortic dissection is a life-threatening condition characterized by a tear in the aortic intima, leading to blood flow between the layers of the aortic wall. It is more common in older males and is associated with HTN, connective tissue disorders, and a history of aortic aneurysms. Typically classified using Standford system of Type A / Type B classification for simplicity. Pathophysiologically, the tear creates a false lumen, disrupting blood flow and potentially causing ischemia. Patients typically present with sudden, severe chest or back pain described as "tearing" or "ripping." On physical exam, findings may include pulse deficits, blood pressure discrepancies, or a new murmur of aortic regurgitation. Diagnosis is confirmed via imaging, with CT angiography being the gold standard. Treatment involves blood pressure control with beta-blockers and emergent surgical intervention for Type A dissections.
Key Terms
- Aortic Dissection
- a tear in the aortic intima.
- Greater Curvature
- Superior portion of aortic arch
- Lesser Curvature
- Interior portion of aortic arch
- Stanford Classification
- Less complex than DeBakey. Type could be Type A, Type B, or Type A and B. Created after Dr. DeBakey created his classification system.
- DeBakey Classification
- More complex than Stanford.
- Type A
- involves the ascending aorta. Stanford classification.
- Type B
- all dissections not invovling the ascending aorta. Standford classification.
- DeBakey Type I
- involves the ascending aorta, aortic arch, and descending aorta.
- DeBakey Type II
- involves the ascending aorta only.
- DeBakey Type III
- involves the descending aorta only.
- DeBakey Type IIIa
- involves the descending aorta distal to the left subclavian artery.
- DeBakey Type IIIb
- involves the descending aorta proximal to the left subclavian artery.
- Acute
- ≤ 14 days
- Subacute
- 15-90 days
- Chronic
- ≥ 90 days
- False Lumen
- True Lumen
- Intramural Hematomes (IMH)
- penetrating aortic ulcers (PAU)
- Re-entry Tears
- Laplace's Law
- wall stress (tension) = pressure * radius
Aortic Dissection Classification
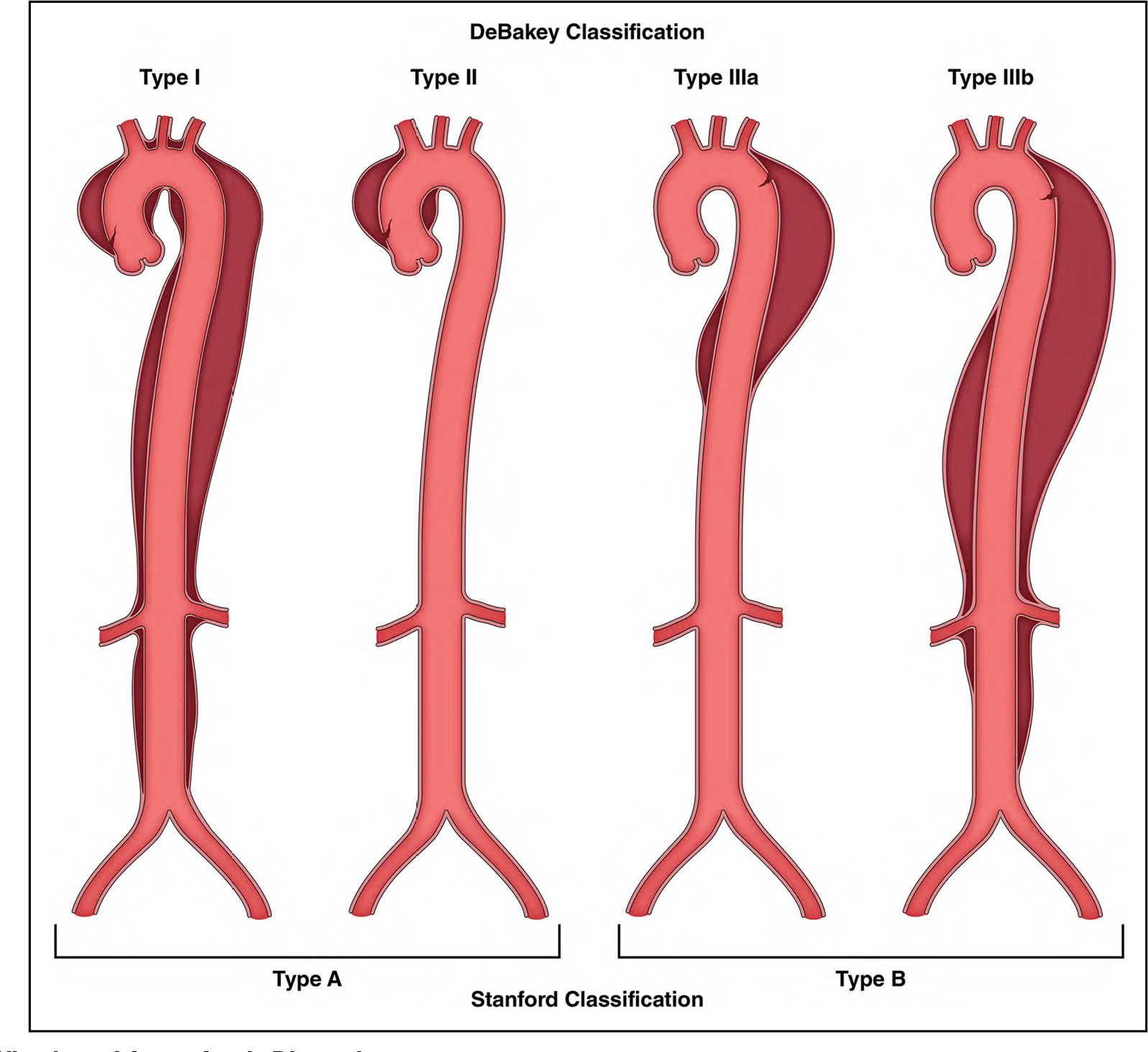
Image Source: Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022;146(24):e334-e482. doi:10.1161/CIR.0000000000001106
Epidemiology
- Risk Factors
- HTN
- Connective tissue disorders
- History of aortic aneurysm
- Connective Tissue Disorders (i.e. Marfan Syndrome)
- Incidence1
- USA 10:10,000
- Increasing d/t better imaging
- Mortaltiy1
- Higher with more complex involvement of aortic structures and poor perfusion of end organs
- 1-3% per hour without surgical repair
- >33% in first 24 hours
- 50% at 48 hours
- 75-90% at 2 weeks
- Survival (with aggressive treatment)1
- 30 day 80-90%
- 50% at 5 years
Etiology
Pathophysiology
- Normal aorta has 3 layers of inside to out: intima, media, and adventitia.
- Normal size: 2- 3 cm in diameter
- A tear in the aortic intima occurs. The aortic layers separate. Prsesurized blood pushes in and creates a false lumen and true lumen. The dissection can grow bigger antegrade or retrograde. Other tears known as re-entry tears can also occur.
Normal Aortic Anatomy
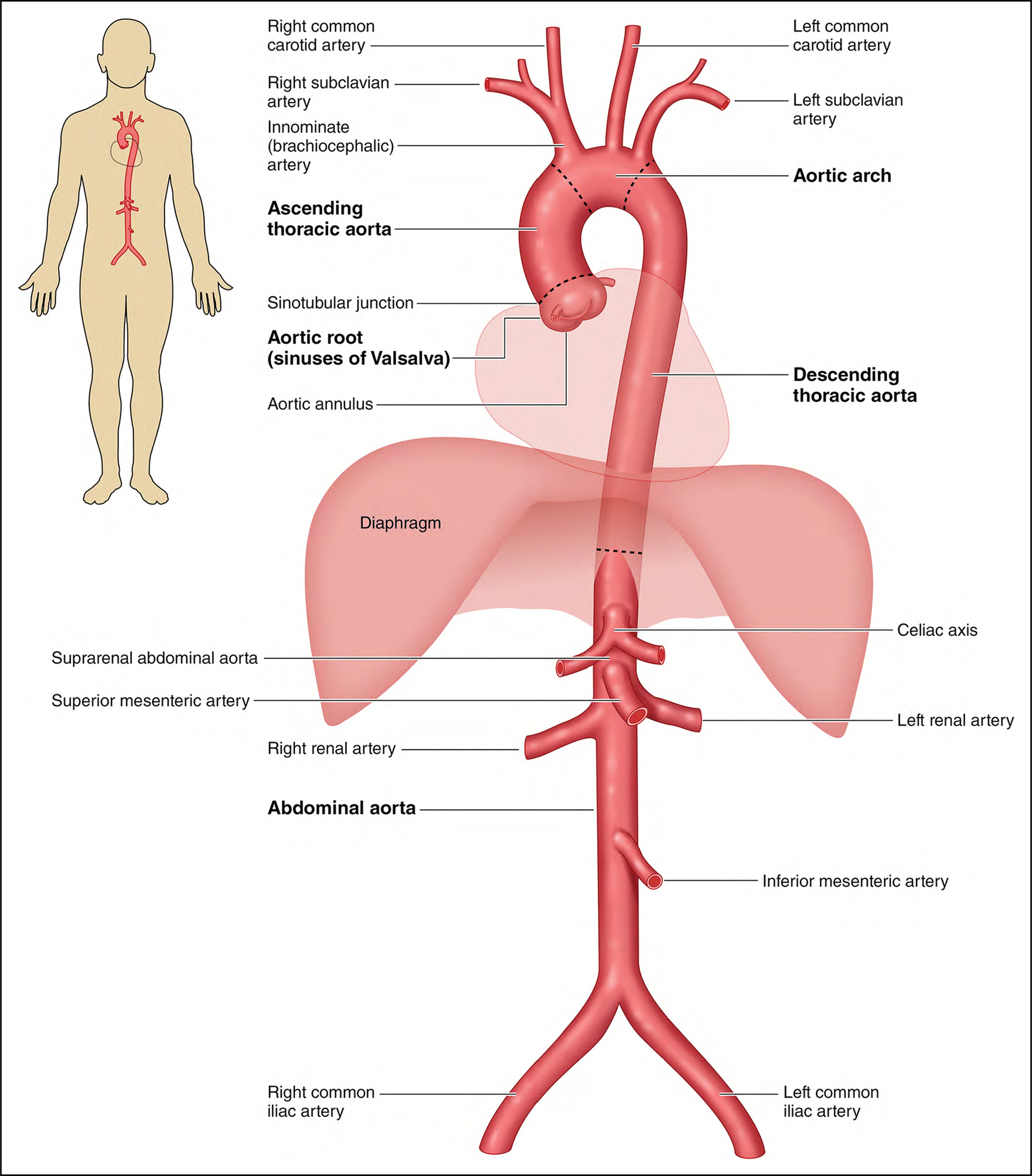
Image Source: Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022;146(24):e334-e482. doi:10.1161/CIR.0000000000001106
HPI
- severe sudden pain
- Midsternal (ascending)
- Interscapular (descending)
- can be painless if aneurysmal aorta
- Tearing or ripping
Physical Exam
- Assess for neurological
Diagnostics
- Note:always look at your own imaging AND ensure measurements of the arch and other structures are performed perpendicular to the aortic axis and not oblique to otherwise this will overestimate the size of the aorta.
- Gold Standard: CTA CTA
- CTA:follow length of aorta assessing for dissection flap, root involvement, aortic branch involement, communicating dissection, intramural hematoma, penetrating atherosclerotic ulcer, focal intimal tear, proximal / distal extension, active contrast extravasation, . In addition, assess for rupture, pericardial fluid.
- TEE:assess valvular involvement, ventricular function, and pericardial / pleural fluid.
Treatment
Prevention
- In pts w/ aortic root or ascending aortic anurysms, screen 1st degree relatives w/ aortic imaging 3-AHA
Referrals
Case Study
Knowledge Check
- What are the branches of the aorta from aortic proximal to distal?
- 1. Brachiocephalic trunk (innominate artery)
- 2. Left common carotid artery
- 3. Left subclavian artery
- What is the most common cause of aortic dissection?
- HTN
- What is the most common presenting symptom of aortic dissection?
- Sudden onset of severe chest or back pain described as "tearing" or "ripping"
- What are the two classifications of aortic dissection?
- Stanford and DeBakey
- What is the difference between Type A and Type B aortic dissection?
- Type A involves the ascending aorta, while Type B does not.
- What is the most common physical exam finding in aortic dissection?
- What is the most important factor in treatment of aortic dissection?
- rapid detection of dissection and transfer of pt to high volume aortic center
- What is the gold standard test of choice for diagnosis of aortic dissection?
- CTA
- Explain how physiologically the false lumen causes malperfusion.
- true lumen collapse d/t force from false lumen compression. In addition, thrombus may form at or near aortic branch ostia statically or dynamically (usually during systole) compromising adequate blood flow to vessel.
References
- TSRA 2nd Edition
- Harvard Natural Sciences Lecture Demonstrations. Laplace's Law and Aneurysms. Accessed Mar 2025.
- Isselbacher EM, Preventza O, Hamilton Black J 3rd, et al. 2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2022;146(24):e334-e482. doi:10.1161/CIR.0000000000001106